There are many studies that associate omega-3 deficiency in the diet with an increase in the risk of cardiovascular disease, cancer, diabetes, neurocognitive impairment and loss of vision.
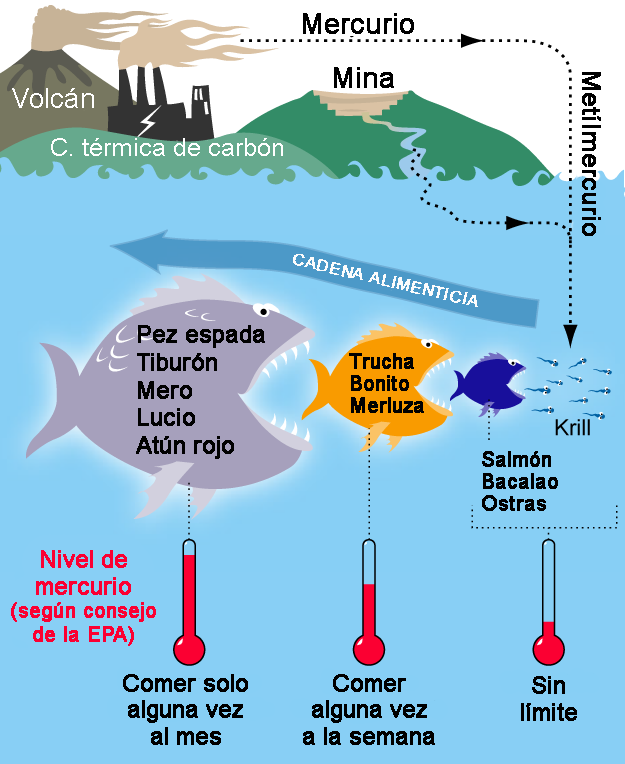
A healthy diet is the basis for a proper nutritional condition, but attaining the appropriate levels of omega-3 isn’t easy. We need to eat oily fish -salmon, sardine, tuna or cod- several times a week, since the rest of the foods rich in omega 3 -bonito, hake, trout, grouper, bluefin tuna, swordfish or shark- contain a high level of heavy metals and there are recommendations when limiting the consumption of fish to prevent their accumulation.
Dr. Iván Moreno – Neolife Medical Team
There are basically two dietary sources of omega-3: one of “marine” origin and the other of “vegetable” origin
Omega-3 fatty acids, in their three variants EPA, DHA and ALA, have been shown to be essential in order for the organism to function properly. Our body can’t produce them and we have to consume them as part of our diet.
There is an abundance of data associating omega-3 deficiency in the diet with an increase in the risk of cardiovascular disease, cancer, diabetes, neurocognitive impairment and loss of vision.
There are basically two dietary sources of omega-3:
- Omega-3 of “marine” origin, mainly eicosapentaenoic acid (EPA) and decosahexaenoic acid (DHA): found in the flesh of oily fish. Also in fish oil and krill oil. They are two long-chain fatty acids that play a fundamentally structural role, becoming part of our membranes.
- The omega-3 of “vegetable” origin is alpha-linoleic acid (ALA): It is found in seeds (Chia), linseed oil, walnuts and green-leafed vegetables. It is a short-chain fatty acid, and unlike the previous ones, our body uses it mostly as fuel.
In recent years the recommendation has been to consume only the omega-3 of vegetable origin, generally for reasons of vegetarianism-veganism. It is not advisable to ingest only one of the two types, since both have shown beneficial effects on the organism (1), and although there are differences between races, on average there is a very low conversion rate of ALA into DHA and EPA (around 0.5-1%). Therefore, no matter how rich our diet is in vegetables and seeds, we will have to consume fish or supplement with marine omega-3.
Consuming fish has many other benefits, containing, as it does, other nutrients in addition to omega-3. Ahealthy diet is the basis for a correct nutritional condition, but to reach adequate levels of omega-3 we need to eat oily fish -like salmon, sardine, tuna or cod- several times a week.
In today’s diets we find ourselves faced with two problems:
- Bad eating habits, due to haste, stress, business commitments, etc., mean that our diet is not as ideal as it should be. We know we should eat better, but impelled by habits or by circumstances we end up eating whatever we have at hand or is easier to get… often processed or precooked food. The first golden rule in achieving good nutrition is to eat real food, cooked in the least aggressive way possible.
- The problem of heavy metal pollution: we’ve been polluting the seas for many years, and unfortunately that pollution is now turning against us. There is a phenomenon involving the accumulation of lead, mercury, cadmium or tin, especially in the largest and most long-lived fish, since they accumulate that of the fish they have been feeding on. Mercury is highly toxic to the body, and there are recommendations when it comes to limiting fish consumption, in order to prevent its accumulation.
How can we tell if we’re getting enough omega-3?
The first thing is to analyze our diet. If we don’t eat fish or we do so very sporadically, it’s very likely that we’re not at the appropriate levels.
Another way of measuring our levels is the Omega-3 Index (O3I). The fatty acids EPA and DHA are destined to become part of our cell membranes, which already gives us an idea of how important it is to consume enough of them. The functioning of our neurons, muscle cells, red blood cells… all of these depend on having a good proportion of EPA and DHA in their membranes.
This is an important idea to bear in mind: fats are not only a fuel that we can “burn” and forget… fats have a structural role and will end up becoming part of us. 60% of our brain is fat, the membranes of our cells are fat… if we eat poorly and consume poor quality fats, it matters little that we exercise a lot to “burn them off”, they will stay with us and will damage our arteries, our brain, our heart, etc.
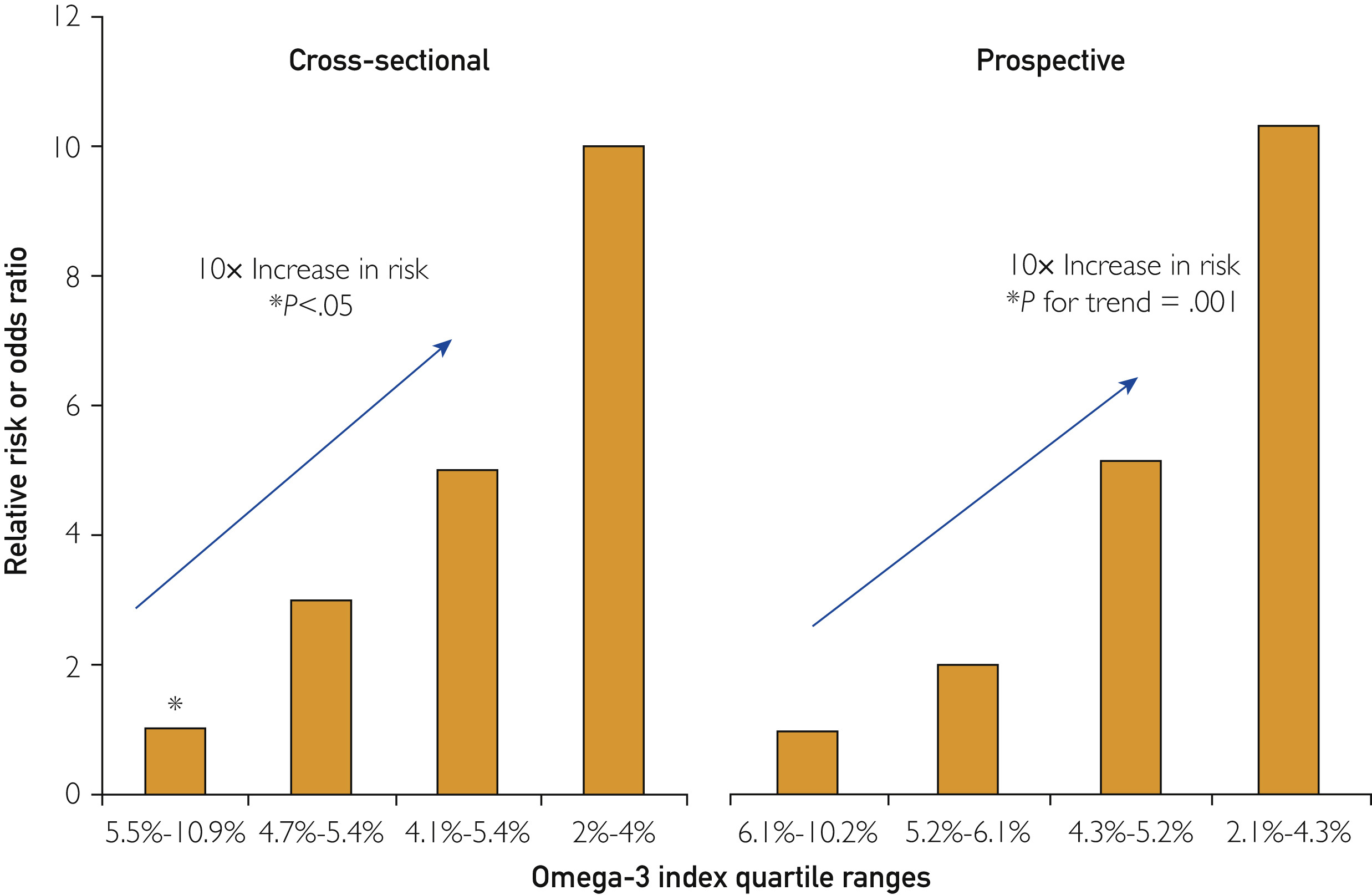
The omega-3 index is calculated by measuring how manyomega-3 fatty acids are in the membranes of our red blood cells and their proportion to the other fats that are found there. And their values are considered:
- Optimum above 8.
- Acceptable between 6 and 8.
- Low between 4 and 6.
- Very low below 4.
It has been shown (2) that those with the highest levels on the omega 3 index presented lower cardiovascular disease (cardiac and cerebral) and mortality. Similarly, patients with a higher O3I were less likely to experience sudden cardiac arrest (3).
Thus, by analyzing our dietary patterns and using the Omega-3 Index we can gain an insight into the specific needs that a person has.
In the same way it’s important to avoid low quality fats, industrial pastries and processed foods that sometimes contain trans-fats, which are directly toxic and should be banned.
Another way to know how good our fat intake is, is by assessing the omega-6 /omega-3 quotient. We need omega-6 fats in our diet, but when they are present in excess compared to the levels of omega-3 they produce more inflammation.
The ideal ratio of omega-6 to omega-3 is 1:1. However, today our average ratio is 20:1 and up to 50:1 due to our diet, which is usually rich in vegetable oils (corn, soybeans, sunflower, evening primrose, egg yolk, etc), and so we should increase the consumption of omega-3 and limit the omega-6 we consume.
Do we need to take supplements?
In our experience, supplementation makes more sense the worse the diet is and the lower the omega-3 index. In a broad meta-analysis summarizing the results of multiple studies and published in the prestigious journal Mayo Clinic Proceedings (4), supplementation with EPA+DHA decreased cardiovascular risk, mainly in patients at a higher risk.
Even so, not everything has been researched, and sometimes conflicting data are found, such as those of the latest review by the Cochrane Library (5), in which they conclude that supplementing in a generalized way doesn’t seem to increase the cardiovascular benefits or improve mortality. Although it may seem striking, this is a phenomenon that we see many times in medicine when performing clinical studies, where actions seem beneficial on paper, but they are applied to individuals without differentiating between those who need them and those who don’t.
Studies don’t usually assess whether participants are eating a good diet, or what their omega-3 index is. They don’t assess whether patients need to supplement with omega-3… it is simply given indiscriminately. This is why the expected benefits sometimes fail to appear among the results of the study.

Supplementing with omega-3 has a special meaning in the case of restrictive diets, where the aim is to try and lose weight, since we can’t restrict fats and achieve a more slender figure at the price of worsening our risk of cardiovascular disease or long-term dementia.

Similarly, there are people who assume that they won’t succeed in finding a diet that is clearly healthy, and prefer to ensure an adequate supply of omega-3. Although the ideal option would be to improve the diet (since it has other added benefits), we need to analyze our situation realistically: it’s hard to achieve a diet that is rich enough. Are we succeeding or would it be better to supplement?
Moreover, in clinical situations where we can’t expose ourselves to more heavy metals or when personal preferences prevent us from consuming meat or animal products, we need to supplement with marine omega-3, since that of vegetable origin doesn’t have the same benefits, and no matter how much we take, our body doesn’t know how to transform one into another.
How to supplement?
One of the problems with supplements is that they have to be properly purified, in order to make sure we get the benefits of EPA/DHA, but not the heavy metals.
In its natural form, krill oil has fewer heavy metals, since it is obtained from bacteria and microorganisms that live in seawater. It tends to be more expensive to buy and in principle doesn’t seem to provide many advantages over fish oil that is well purified. Nonetheless, it is an option for people who don’t want to ingest products of animal origin for whatever reason.
To reach the optimal values on the O3I, it is recommended to consume around 100 g of oily fish daily (look for sources with few heavy metals) or take a good omega 3 supplement that provides sufficient amounts of:
- DHA – between 0.5 and 1 g.
- EPA – between 0.75 and 1.5 g.
In short, we could sum up by remembering that we need to avoid having a deficit of omega-3, which has been associated with numerous health problems, and that, although diet is the fundamental source, when ours is poor or for other reasons we won’t be able to make sure we get enough, it’s better to supplement with adequate levels.
At Neolife we practice personalized medicine, while avoiding indiscriminate supplementation and adjusting the supplements to the needs of each patient. After analyzing your diet, and depending on each case -also assessing the omega-3 index-, we’ll advise you on what your body needs.
BIBLIOGRAPHY
(1) MD AMF, MD PBM, MD KA, PhD NFGM, MD NDB, MD CBE, et al. A Clinician’s Guide for Trending Cardiovascular Nutrition Controversies. Journal of the American College of Cardiology. Elsevier; 2018 Jul 31;72(5):553–68.
(2) Harris WS, Tintle NL, Etherton MR, Vasan RS. Erythrocyte long-chain omega-3 fatty acid levels are inversely associated with mortality and with incident cardiovascular disease: The Framingham Heart Study. Journal of Clinical Lipidology. 2018 May;12(3):718–727.e6.
(3) MD JHO, MD DJ, MD CJL. Omega-3 Fatty Acid Therapy: The Tide Turns for a Fish Story. Mayo Clin Proc. Mayo Foundation for Medical Education and Research; 2017 Jan 1;92(1):1–3.
(4) MSPH DDAP, RD PEMPM, Van Elswyk PhD RD ME, RD CNKP, MPH LCB. A Meta-Analysis of Randomized Controlled Trials and Prospective Cohort Studies of Eicosapentaenoic and Docosahexaenoic Long-Chain Omega-3 Fatty Acids and Coronary Heart Disease Risk. Mayo Clin Proc. Mayo Foundation for Medical Education and Research; 2017 Jan 1;92(1):15–29.
(5) Abdelhamid AS, Brown TJ, Brainard JS, Biswas P, Thorpe GC, Moore HJ, et al. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Heart Group, editor. Cochrane Database of Systematic Reviews. 2018 Jul 18;304(17):1903–743.
