By early 2021, CoV-2 has already infected over 90 million people and claimed the lives of nearly 2 million others worldwide. Vaccination is the only tool that can effectively stop the virus from spreading and eradicate the pandemic.
Currently, two vaccines are available: the one developed by Pfizer-BioNTech and the one developed by Moderna. Both vaccines are included within the mRNA group. But how do these vaccines work? What types of vaccines are there? And how did we manage to have an effective and safe vaccine in record time?
Dr. Débora Nuevo Ejeda – Neolife Medical Team
Our line of defense against infection: THE IMMUNE SYSTEM
To understand how vaccines work, it is essential to first understand our immune system’s mechanism for action.

In broad terms, we could say that white blood cells or leukocytes are responsible for our body’s defenses. Likewise, in a simple way we may differentiate three different types of white cells with a primary role in defending our body from infection:
- Macrophages: This type of white blood cell surrounds microorganisms and destroys them, extracting some particles (called antigens) that stimulate the action of other components of the immune system.
- B cells: These white cells are responsible for humoral immunity. They secrete antibodies that recognize antigenic molecules. Another function is to present these antigens to T cells and in this way regulate the inflammatory response.
- T cells: These are white blood cells that specialize in cellular immune response, which is primarily directed at organisms that replicate within the cell (such as viruses).
When we first come into contact with CoV-2, it can take weeks for our body to trigger and effectively use all these strategies to fight the virus. However, if we encounter the same virus again, memory T cells start working quickly, and B cells recognize the antigens they are already familiar with and begin to produce antibodies directed against the attacker.
How do vaccines work? What types of COVID vaccines are currently available?
Vaccines help this entire process develop easily and quickly without the need for a previous infection.
There are currently three types of coronavirus vaccines that are already available or in phase 3:
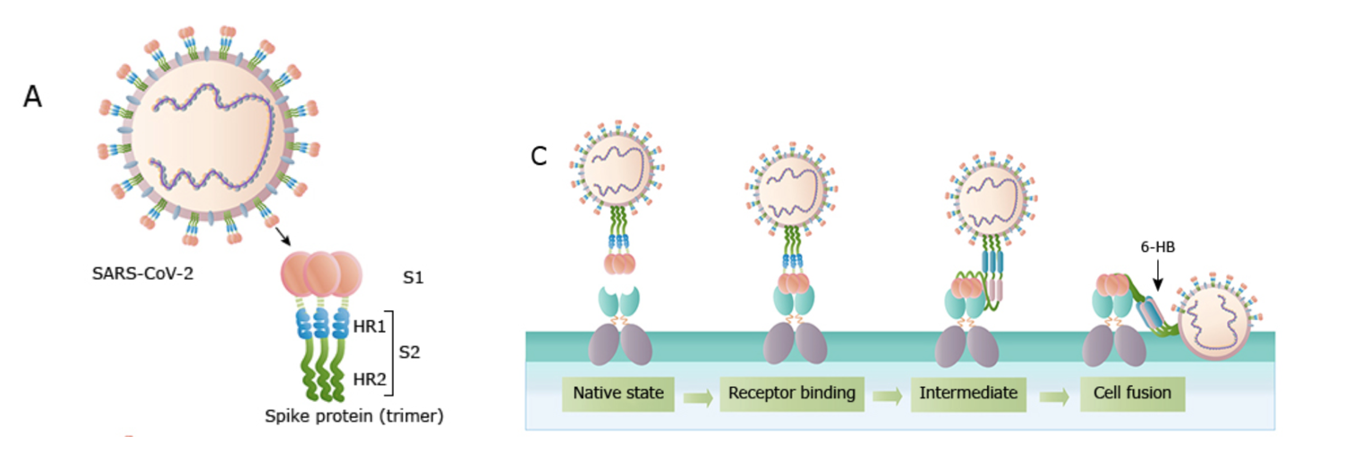
- MRNA vaccines: This is a type of vaccine that instructs our cells to make a protein that is unique to the virus. In fact, it contains a small part of the genetic code that teaches our cells to manufacture a protein, called “spike protein“, which is normally located on the surface of the virus and helps the virus attach itself to our cells and enter them. This protein is specifically recognized by our immune system as a foreign invader, and so it begins to produce antibodies, as if we had come into contact with the virus causing the infection. But this vaccine in no way, shape, or form contains the virus itself or any part of it.
- Protein subunit vaccines: These vaccines contain the harmless proteins of the virus, but not the virus itself. As with the above, our body detects these foreign proteins and begins to create T cells and antibodies. This way, if we are infected in the future, the memory cells recognize the virus and trigger the learned immune response.
- Viral vector vaccines: These vaccines are based on often different and attenuated versions of a live virus, which contains CoV-2 genetic material (this is called a viral vector). Once this viral vector has entered our cells, it instructs them to produce a protein that is unique to the coronavirus, against which our body begins to manufacture T and B cells, which would be ready to attack if we became infected in the future.
Currently, the two vaccines available (the Pfizer and the Moderna vaccines) are both of the first type: mRNA vaccines. It is a fairly new type of vaccine, although they have been studied for a long time. Their completely in vitro production allows them to be produced in large quantities, although their need for storage at low temperatures somewhat complicates their distribution.
Vaccine development
Vaccines undergo three stages (Phase I, Phase II, and Phase III) in their development. These steps occur sequentially, and each step usually takes several years to complete. In the case of the COVID vaccines, this process was accelerated in an unprecedented way, so that steps that lasted for years were completed in just a few months. Even so, the safety criteria have remained intact.
The process of creating vaccines has been the following:
- Preclinical trials: Initial vaccine candidates are administered in animals (typically mice), and the resulting immune response is measured. To continue towards the next phases, an adequate immune response must be generated, but its safety must also be tested in animals. In the case of the COVID vaccine, it was also administered and studied in non-human primates at this stage.
- Phase I clinical trials: Pre-vaccines that have generated an immune response without animal toxicity advance to human trials. Usually 100 or fewer healthy subjects are chosen. The fundamental goal of this phase is to test the safety of the experimental vaccine, although its immunogenicity is also tested. The dose ranges are also investigated in this step. The first subjects receive small doses, and these are increased in the following subjects to receive it. Possible side effects, both local and systemic, are monitored very thoroughly and on a daily basis. Fever, swelling, and redness of the skin at the injection site, as well as other more serious reactions that may interfere with normal activity, are monitored daily.
- Phase II clinical trials: The goal here is to ensure the efficacy and effectiveness of the immune response in a wider number of subjects, usually several hundred. In the case of COVID-19 vaccine studies, Phases I and II and Phases II and III were combined without a phased transition between phases.
- Phase III clinical trials: At this stage, subjects are assigned randomly and blindly, either to a control group that receives a placebo or to the group receiving the vaccine. The goal is to assess the effectiveness of the vaccine in reducing the incidence of the disease. The following formula is used: (attack rate in unvaccinated – attack rate in vaccinated / attack rate in unvaccinated x 100).
Pfizer (BNT162b2) vaccine
It is an mRNA vaccine developed in a lipid nanoparticle that contains instructions for expressing the spike protein in its full length.
There are two separate doses, 21 days apart, given in an intramuscular injection into the upper arm.
It is suitable for individuals over 16.
Clinical trials registered 95% effectiveness in preventing laboratory-confirmed COVID-19cases in individuals with no evidence of previous infection.
Most of the side effects observed were mild or moderate. The most common effects were localized: pain, swelling, and redness in the arm where the vaccine was injected, and usually within the first seven days after administration. The most common general side effects include chills, headache, and tiredness, and were more common after receiving the second dose.
Moderna (mRNA-1273) vaccine
This vaccine was one of the first SARS-CoV-2 vaccines to be produced. It was developed and administered in humans only two months after the publication of the genomic sequencing SARS-CoV-2.
Just as the Pzifer vaccine, it is included in the mRNA vaccine group and was developed into a lipid nanoparticle where the mRNA is found to express the spike protein in its full length.
The way it is administered is the same: two intramuscular injections applied to the upper arm, this time one month apart (28 days).
Indicated for individuals over 18, its side effects are the same as those for the vaccine developed by Pfizer.
Its effectiveness in clinical trials was registered at 94.1% in the prevention of laboratory-confirmed COVID-19 cases in individuals who received two doses and did not present a history of previous infection.
Both vaccines are discouraged in:
- Patients with a severe allergic reaction (anaphylaxis) or an immediate allergic reaction, even if not severe (within 4 hours after vaccination, and with symptoms such as hives, swelling, or wheezing) to any of the components of the mRNA vaccine against COVID-19.
- Patients who have a severe or immediate allergic reaction should also not receive the second dose of the vaccine after receiving the first dose.
- Special consideration for pregnant women: Safety data for COVID-19 vaccines in pregnant women and breastfeeding women are limited, simply because they have not been studied. However, it is believed that they are unlikely to present a particular risk.
Which vaccines are coming soon?
Currently, several vaccines are already in Phase III, and their approval for distribution and administration in the general population is expected to come in a very short period of time.
Unlike the two available at the time of writing this blog post, the upcoming vaccines are protein subunit vaccines or viral vector vaccines, the kind that use attenuated versions of the virus.
- Novavax (NVX-CoV2373): protein subunit vaccine containing spike glycoprotein. It is also administered in two intramuscular doses, 21 days apart.
- University of Oxford, AstraZeneca, and Serum Institute of India (ChAdOx1 nCoV-19/AZD1222): This vaccine uses a chimpanzee adenovirus as a vector to express the spike protein and trigger the same immune response. The first dose is administered intramuscularly and after 28 days the need for a second dose would be evaluated.
- Janssen (Ad26.COV2.S): Like the previous, it is a vaccine that uses an adenovirus as a vector to express a stable spike protein. This vaccine appears to be able to neutralize the virus and produce antibodies after a single intramuscular dose.
- Gamaleya Institute (Sputnik V): This Russian vaccine also uses the replication of an adenovirus to produce a full-length spike protein. It is also administered in two intramuscular doses, 28 days apart.
- Sinopharm (BBIBP): This vaccine belongs to the group of attenuated virus vaccines.
It uses a chemically inactivated version of SARS-CoV-2. Administration is intramuscular and repeated after 28 days. - Sinovac (coronaVac): Like its Chinese colleague Sinopharm, this lab has created a vaccine with an inactivated SARS_CoV-2 virus for intramuscular administration in 2 separate doses 28 days apart.
BIBLIOGRAPHY
(1) Merryn Vpysey, DOhil, Suw Ann Costa Clements, PhD, Dhabir A Madhi, PhD, LylyY Weckx, PhD, Pedro M Folegatti, MD, Pravinder K Aley, PhD et al. (2021). Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021;397; 99-11. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)32661-1/fulltext
(2) Kathryn M Edwards, MD, Walter A Orenstein, MD. ( 2021) Coronavirus disease 2019 (COVID-19): Vaccines to prevent SARS-CoV-2 infection. In martin S Hirsch, MD (Ed), , (UpToDate) https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-vaccines-to-prevent-sars-cov-2-infection?
(3) World Health Organization. Draft landscape of COVID-19 candidate vaccines. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
