We live in mutualistic symbiosis with these microorganisms that inhabit our gut; we need each other.
Having a healthy microbiota is vital for our mental health, weight and appetite control, rest, lowering our cardiovascular risk, lowering our risk of developing diabetes, lowering our risk of developing cancer, having a proper immunity, preventing the development of autoimmune diseases, intolerances, allergies, migraine, diarrhea, constipation and abdominal pain, infertility, etc…
Dr. Alfonso Galán González – Neolife Medical Team
The microbiota is of utmost importance to our immune system.
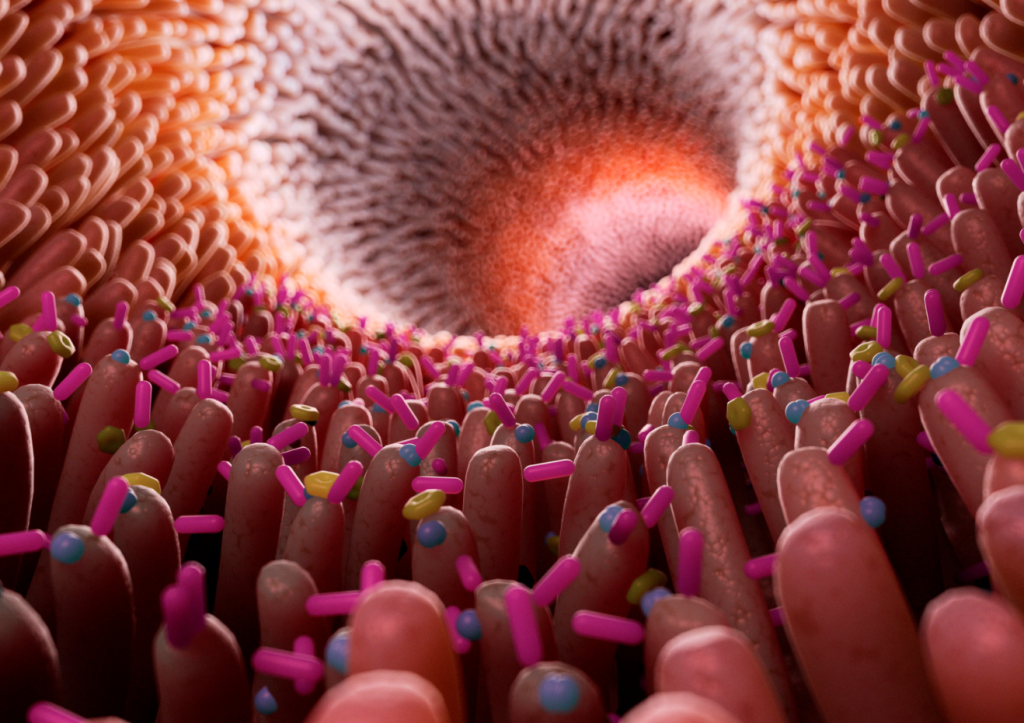
You may know it as gut microbiota, microbiome, or gut flora in more colloquial terms. By now, we all know that we have healthy bacteria in our intestine that live with us and provide beneficial effects to our bodies. But do you really know how important they are? Did you know that changes in our microbiota are linked to pathologies? Did you know that we can study it…and repair it?
We also have microbiota in our skin and mucous membranes in physiological terms (except for the conjunctiva of the eye, which is sterile by definition). Approximately 80% of our immune system cells are in the gut and communicate via blood and lymph with the rest of the body.
Our gut microbiota accompanies us from the moment we are born (some studies now suggest that the amniotic fluid in which we swim before birth already carries bacteria that begin to populate our gut). As we pass through the birth canal, lay on our mother’s breast, receive kisses from family members, and suckle for the first time, we receive bacteria that colonize our gut. Our flora matures during the first 4-5 years of life, as we are exposed to different environments and foods.
Symbiosis and health
We live in mutualistic symbiosis with these microorganisms; we need each other. And we say microorganisms because they are not only bacteria, but also fungi and yeasts, viruses, protozoa, and archaea.
Some interesting facts:
- We have 100 trillion bacteria in our gut. This is 10 times more than the number of cells in the entire body!
- We have more than 1000 different species of bacteria.
- About 2 kg of our body weight is comprised of microbiota.
- They make up 48% of the weight of our stool.
- Our body is comprised of 21% protein, and we are not able to synthesize many amino acids (the components of proteins), but our microbiota can.
- More than 30% of the substances circulating in our blood are produced by the microbiota.
Our microbiota need multi-species communities to live and complete their metabolic capacity to degrade nutrients, obtain energy, and synthesize essential compounds for the community.
Having a healthy microbiota is vital for our mental health, weight and appetite control, rest, lowering our cardiovascular risk, lowering our risk of developing diabetes, lowering our risk of developing cancer, having a proper immunity, preventing the development of autoimmune diseases, intolerances, allergies, migraine, diarrhea, constipation and abdominal pain, infertility, etc…
I hope I got your attention with this last paragraph. Everything it says has been rigorously and scientifically proven, and, as always, we will get into it in greater detail.
The microbiota is of utmost importance to our immune system; 80% of our immune system cells are in the gut and communicate via blood and lymph with the rest of the body. It influences the maturation and correct functioning of our immune system by “training” it continuously and teaching it what to attack and what not to attack.
It constitutes a physical and biochemical barrier to prevent the entry of pathogens. If our microbiota is not in balance, we enter into what we call dysbiosis which leads to inflammation and disease.
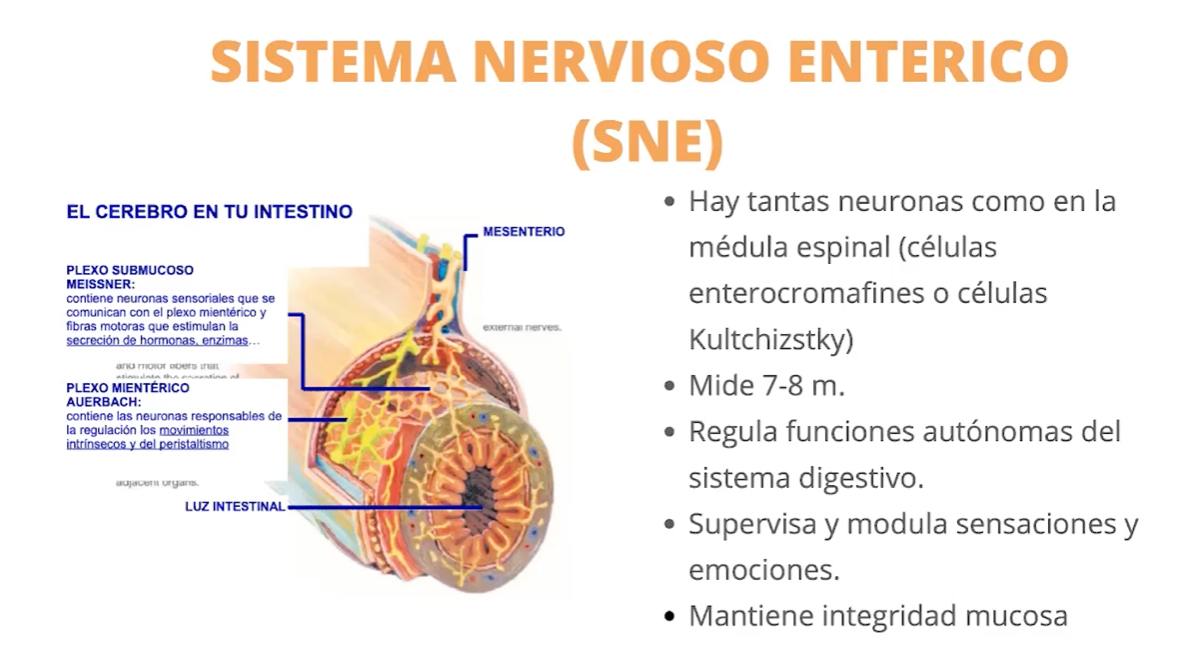
It behaves like a real “second brain”. The enteric nervous system contains as many neurons as our medulla. Sixty percent of the information that reaches our brain comes from our gut, and it produces neurotransmitters in even greater quantities than the central nervous system (CNS). With our CNS, it is permanently in communication through these neurotransmitters, the hypothalamic-pituitary-adrenal axis (which we covered here), the bacterial metabolites, and cytokines secreted, etc… Who hasn’t felt nervousness, fear, hope, all kinds of emotions in “the gut”? They are closely related.
Functional groups
The most important and most studied group of gut microbiota are bacteria. As already mentioned, there are over 1000 species that are grouped into a number of functional groups, with similar functions. This facilitates their study and analysis.
We should make a distinction between the group of medium stabilizing bacteria and the group of facultative pathogens. Within the group of those that control the stability and homeostasis of the intestinal environment, we find bacteria that are protective, immunomodulatory, muconutritive, primary saccharolytic, and neuroactive. We’ll discuss their functions and the consequences of their alteration below.
Among the facultative pathogenic microorganisms, we find proteolytic bacteria, and fungi and yeasts.
The following depend on the functional stability of our microbiota:
- Food digestion
- The absorption of nutrients
- Normal immune, metabolic, and neuroactive performance
Immunoregulatory Microbiota
The most important bacteria in this group are apathogenic Escherichia coli and Enterococcus faecalis.
They locally regulate all the components involved in immune response, ensure a continuous training of the immune system, are able to induce non-specific immune responses, and collaborate with the immune system in the phenomena of immune identification or immunotolerance (identifying pathogens as pathogens and harmless molecules as non-pathogenic and therefore not susceptible in order initiate the correct immune reaction).
If we have a test result that shows a level that is below the normal range for these bacteria, the subject has an increased susceptibility to immune disorders such as autoimmune diseases, allergies, or immunodeficiencies.
Protective Microbiota
These are mainly bacteria like as Lactobacillus, Bifidobacterium and Bacteroides.
They stabilize the intestinal environment by maintaining the necessary acid pH in the intestine, and synthesize bacteriocins and hydrogen peroxide, protecting us from the growth and colonization of pathogenic microorganisms. Additionally, they strengthen and repair tight junctions, the junctions between the cells of the intestinal epithelium; when these fail, they lead to the very common symptoms of intestinal permeability.
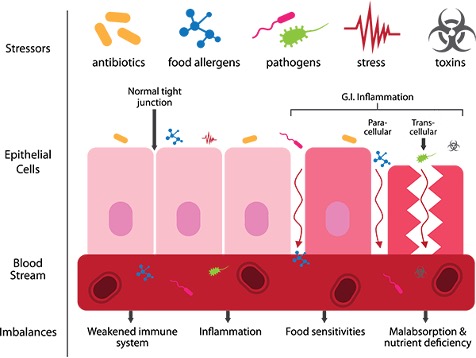
If their number is low, we lose this barrier function against pathogens; the environment is destabilized, favoring dysbiosis, and nutrient absorption is compromised.
Muconutritive Microbiota
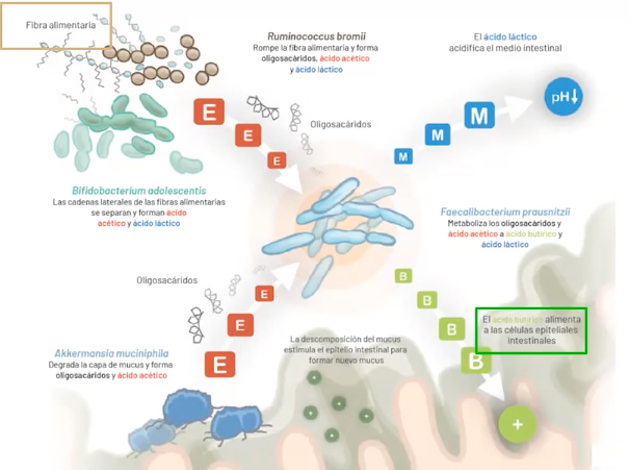
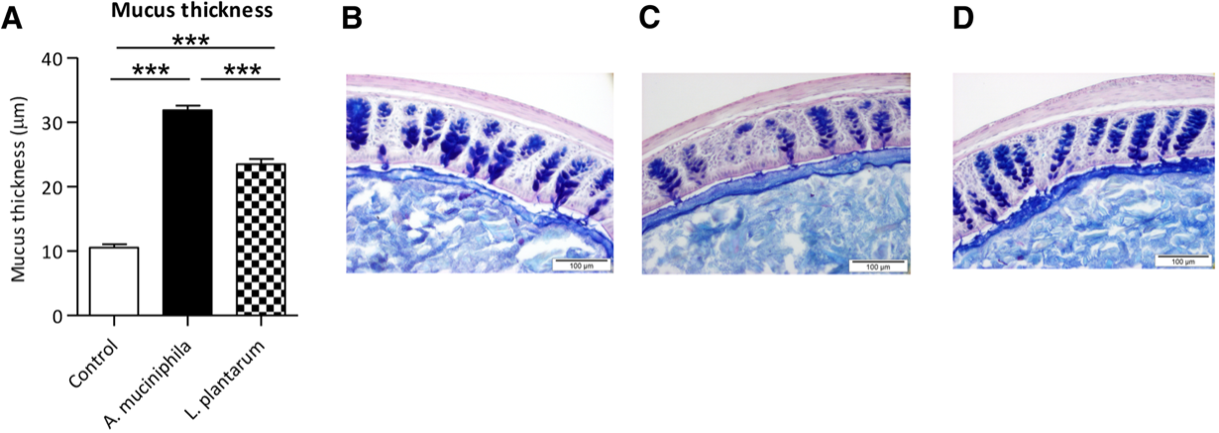
The most important bacteria in this group are Faecalibacteroium prausnitzii and Akkermansia muciniphila.
They stabilize the mucus layer that lines the intestinal epithelium, where our microbiota lives. They renew this mucus layer by degrading it and the intestinal fiber, producing oligosaccharides and SCFA (short-chain fatty acids) that serve as food for the intestinal cells and the rest of the microbiota. They modulate inflammation, and in a very important and characteristic way, they regulate neoglycogenesis, that is, the synthesis of glucose in the liver.
When these bacteria are low, we have an increased susceptibility to suffer from inflammatory pathologies such as Crohn’s disease and ulcerative colitis, and metabolic diseases such as type 2 diabetes, metabolic syndrome, obesity, or non-alcoholic fatty liver disease.
Primary saccharolytic Microbiota
The most important bacteria in this group are Bifidobacterium adolescentis and Ruminococcus Bromii
They support muconutritive microbiota in the digestion of long and complex carbohydrate chains. They stimulate other species to degrade dietary fiber normally. They are essential for the primary degradation of resistant starch and oligofructose, producing butyric and lactic acid that nourish intestinal cells and acidify the medium respectively.
A low count in this functional group, therefore, means that we cannot digest complex carbohydrates well and do not effectively produce the aforementioned SCFA.
Neuroactive Microbiota
Once again, Bifidobacterium adolescentis and lactobacillus plantarum are the most important bacteria in this group.
Neuroactive microbiota are able to synthesize GABA (Gamma amino butyric acid), which is an essential neurotransmitter especially in cases of anxiety. They also modulate neurotransmitter receptors and stabilize the gut-brain axis, the immune system, and visceral pain. Their ability to synthesize neurotransmitters like those in our brain means that our bacteria and our brain have a common language that functionally consolidates this gut-brain axis. We know that by administering Lactobacillus plantarum to stressed individuals, their stress and anxiety is reduced, with a correlation in the levels of neurotransmitters like GABA, serotonin, dopamine, and norepinephrine. Depressed patients show intestinal dysbiosis and alterations in neurotransmitter levels, affecting the gut-brain axis.
Proteolytic Microbiota
Proteolytic microbiota is composed of various bacteria that are facultative pathogens. That is, in the right balance and quantity, they do favorable work for the host, but if they get out of control, they can harm us.
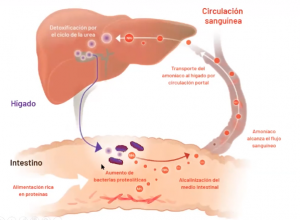
They contribute to the digestion of proteins by generating good degradation products such as amino acids, and potentially harmful ones such as biogenic amines (some known as histamine and others with disturbing names like putrescine or cadaverine), ammonia, etc….
If we have an overgrowth of proteolytic bacteria, the pH of the intestine – which, remember, should be physiologically acidic – becomes more alkaline, favoring the development of pathogens. Our system tries to acidify the intestine again at the cost of overloading the liver and consuming our blood bicarbonate, leading to further acidification of the environment. These proteolytic bacteria injure the intestinal mucosa producing chronic inflammation and altering intestinal permeability.
Fungal Microbiota
Composed of fungi and yeasts, the most important of these is Candida.. If it grows above normal levels, it becomes pathogenic and releases toxic metabolites; it may also behave as a reservoir of fungi so that we may present infections in other areas such as the mouth (thrush), vagina (yeast infection), etc.
Well, I hope this has conveyed just how important it is to have a balanced microbiota, where we have the right amount of all the bacteria and microorganisms necessary, without an overgrowth of facultative pathogens or a weak protective microbiota.
Environmental and toxic factors
Unfortunately, the life we live may lead us to a real extinction of our intestinal bacteria, favoring cases of dysbiosis.
These are just a few of the external factors that may affect you:
- Diet; an excess of meat, sugar, or low fiber intake alter our flora.
- A sedentary lifestyle favors dysbiosis.
- Rest; circadian rhythm disorders and deregulation also favor dysbiosis.
- Chemicals; from additives to endocrine disruptors, these alter our gut bacteria.
- Drugs; especially antibiotics and proton pump inhibitors (the famous Omeprazole and drugs of that family).
- The very same aging process is related to a decrease in the population of protective bacteria and an increase in proteolytic bacteria.
It is more than likely that you have identified with one or more of these symptoms, which may be an indication of an imbalance in your microbiota.
At Neolife, we may now assess your intestinal microenvironment in the most scientific and advanced way with a simple stool sample. Our medical team will correlate your symptoms to the test findings and propose the best way to restore balance in your microbiota and correct the problem.
BIBLIOGRAFÍA
(1) Role of the normal gut microbiota. World J Gastroenterol 2015 August 7; 21(29): 8787-8803
(2) Enterococcus faecalis Inhibits Hyphal Morphogenesis and Virulence of Candida albicans Melissa R. Cruz, Carrie E. Graham, Bryce C. Gagliano, Michael C. Lorenz, Danielle A. Garsin Infection and Immunity January 2013 Volume 81 Number 1. 189-200
(3) Review Article: Association between Faecalibacterium prausnitzii Reduction and Inflammatory Bowel Disease: A Meta-Analysis and Systematic Review of the Literature Hindawi Publishing Corporation Gastroenterology Research and Practice Volume 2014, Article ID 872725, 7 pages
(4) Exploring the influence of the gut microbiota and probiotics on health: a symposium report Linda V. Thomas, Theo Ockhuizen and Kaori Suzuki. British Journal of Nutrition (2014), 112(S1), S1–S18
(5) Role of the Microbiota in Immunity and Inflammation Yasmine Belkaid and Timothy W. Hand Cell 157, March 27, 2014 ª2014 Elsevier Inc. 121-141
(6) Contribución de la microbiota intestinal y del género «Bifidobacterium» a los mecanismos de defensa del huésped frente a patógenos gastrointestinales Y. Sanz, M.C. Collado, J. Dalmau Acta Pediatr Esp. 2006; 64: 74-78
(7) Probiotics and prebiotics and health in ageing populations Sylvia H. Duncan∗, Harry J. Flint Maturitas 75 (2013) 44– 50