Low testosterone levels can lead to weight gain and an increase in visceral fat, whilst obesity, in turn, can lead to a decrease in testosterone levels.
The relationship between obesity and testosterone deficiency is, therefore, bidirectional. And both factors correlate with the onset of cardiovascular diseases, oncological diseases and an increase in overall mortality. Are there any solutions? Follow a personalized and effective nutritional program that ensures you do not stray into obesity, as well as a bioidentical hormone treatment that will restore low testosterone levels to a normal level once again.
Dr. Moisés De Vicente – Neolife Medical Team
Testosterone deficiency and general obesity correlate to an increase in mortality independent of each other but there is also an inversely proportional relationship between them.
A homeostatic balance is one of the fundamental elements necessary for us to age gradually and maintain our quality of life. To achieve this it is necessary to ensure our body is ready, as if the body was a clock. Two of the pillars on which we must focus are obesity and hormonal imbalance.
The overweight epidemic suffered in most developed countries is well known to all of us. Our lifestyles and diet have lead us, inexorably, to the weight we all gain at some point in our lives and, in some cases, some of us appear to gain weight indefinitely. But this increase in weight does not only imply a physical deterioration. Obesity is clearly related to the onset of cardiovascular and oncological diseases and an increase in mortality risk (1).
On the other hand, a hormonal deficiency typically begins to present in people aged 35-40. In the case of men, this decline is typically associated with a decrease in testosterone levels. It has been estimated that up to 38.7% of men have insufficient testosterone levels by the age of 45.
Testosterone acts in a number of basic physiological events within our body. Not only does testosterone improve physical activity and sexual quality, but it also acts on muscle development allowing us to maintain an adequate weight and even prevent cognitive deterioration (2). As with obesity, a decline in testosterone is related to the onset of cardiovascular and oncological diseases and with an increase in overall mortality (3).
Such evidence when viewed in isolation warrants a special mention irrespective of the correlation which is known to exist. It is for this reason we consider it interesting how these two conditions do not seem unrelated. There is an inversely proportional relationship between the onset of obesity and testosterone deficiency. But, let us not forget this relationship is also bidirectional. That is to say, on the one hand, low testosterone levels can lead to weight gain and an increase in visceral fat whilst, on the other hand, obesity can lead to a decrease in testosterone levels (4). Now, the reason for this dualism is something that has not been clarified to date.
It is conjecture at this time that the presence of these two conditions increases the mortality even more than they would independently. For this reason, a study published in Clinical Endocrinology has been designed to answer this question directly.
The study included more than 1,500 men aged 20 and over who did not have any known cardiovascular disease or prostate cancer. During the study testosterone levels in the blood were taken. Participants were also given a nutritional questionnaire and their weight, height and abdominal girth were measured before their body mass index was calculated. A follow-up was conducted 9.5 years later.
The results confirmed what had already been demonstrated in other publications: that a testosterone deficiency by itself, and independent of other variables could be linked to a higher mortality risk. Likewise, the presence of this deficiency has also been associated with abdominal obesity, which in turn has been shown to correlate with an increase in mortality (Figure 1).
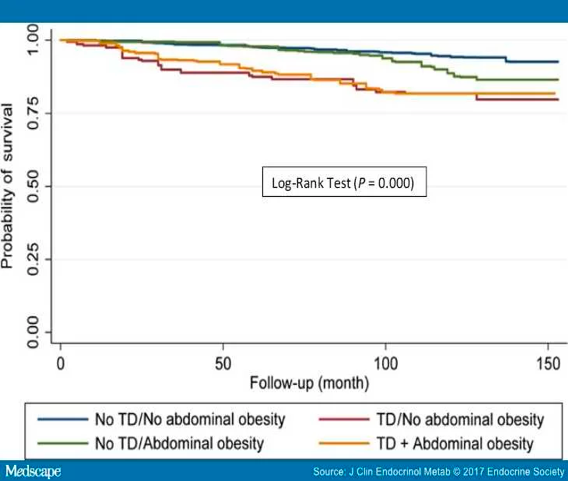
However, the relationship between testosterone deficiency and general obesity has not yet reached a sufficient level to be able to categorically confirm that chances of survival decrease as a result of the relationship. As it has been published in different studies, it seems that testosterone acts mainly on visceral fat, which typically manifests in the presentation of abdominal obesity. And it is this visceral fat that could be responsible for the onset of the different pathologies listed at the beginning of the article. As a result, we can now understand that the relationship that clearly links to the deaths is this, and not general obesity.
In light of these results, it is evident that the cocktail of testosterone deficiency and abdominal obesity is dangerous and we should focus our efforts on correcting the underlying issues. And here is where we discover another important element: correcting only one of the issues in isolation may not be enough to achieve the desired objective. In the long term, an unresolved testosterone deficiency will make it increasingly difficult to lose weight, and this, in turn, will increase the testosterone deficiency.
This then creates a vicious circle that is very difficult to break with conventional medicine. Taking into account that mortality is greater if a patient presents with these two characteristics, it is essential that we take steps to shuffle the deck in some way. And sometimes, to shuffle the deck it is necessary to put a fist through the table.
At Neolife we push against the obesity trend by encouraging patients to adhere to a program of personalized nutrition and many achieve excellent results. In addition to this, we are pioneers in the use of hormone treatment using bioidentical hormones. We carry out a comprehensive assessment and measure testosterone levels and rebalance the latter where necessary.
Thanks to this program -where we use different strategies, but all of them perfectly connected-, we are able not only to improve the quality of life of our patients, but also to decrease their mortality risk. By utilizing this program we are able to get our patients to take a key step towards breaking the deadly cocktail.
BIBLIOGRAPHY
(1) Global BMI Mortality Collaboration, Mortality C, Di Angelantonio E, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388:776–786.
(2) Khera M, Adaikan G, Buvat J, et al. Diagnosis and treatment of testosterone deficiency: recommendations from the fourth international consultation for sexual medicine (ICSM 2015). J Sex Med. 2016;13:1787–1804.
(3) Platz EA. Low testosterone and risk of premature death in older men: analytical and preanalytical issues in measuring circulating testosterone. Clin Chem. 2008;54:1110–1112.
(4) Kelly DM, Jones TH. Testosterone and obesity. Obes Rev. 2015; 16:581–606.
