Obesity is a growing epidemic and one of the leading causes of preventable death worldwide. Unhealthy eating habits and a sedentary lifestyle are most responsible for weight gain and fat accumulation.
Obesity is a disease that affects over 650 million people worldwide. It’s a global public health problem, and it costs over 150 billion annually to treat acute and chronic obesity conditions. Recently, a promising study has been published, which has demonstrated the action mechanism and preclinical efficacy of a protein called BAM15, effective in the treatment of obesity and related metabolic disorders.
Alejandro Monzó – Neolife Nutrition and Nursing Unit
BAM15 is a protein that prevents weight gain and fat accumulation, while reducing blood sugar levels
Advances in small molecule screening and biochemical engineering have led to a renewed interest in mitochondrial agents directed towards the treatment of metabolic disease, such as obesity. Currently, only four medicines (orlistat, phentermine-topiramate, naltrexone-bupropion, and liraglutide) are approved for the treatment of obesity (2, 3). However, they are limited when it comes to effectively providing long-term weight loss.
Their limitations are due, in part, to the difficulty in identifying bioactive compounds with a wide therapeutic range that address the multifactorial causes and effects of obesity. Recently, the scientific journal EMBO Molecular Medicine published research that reveals a very promising step in addressing obesity. The protein BAM15, a mitochondrial proton translocator, may be used to treat this chronic, non-communicable disease (3).
In general, existing medications work by reducing appetite or calories absorbed after food intake (2). The protein BAM15 differs greatly from these drugs, as its potential lies in decreasing the efficiency of cellular mitochondria, resulting in their “burning” more energy (3). Mitochondria are the cellular organelles responsible for supplying most of the energy needed for cellular activity, acting as power plants and releasing ATP, which is the fuel for most cellular processes (4).
Researchers have shown in trials with mice that those who received BAM15 burned more calories and therefore had a lower weight gain than the mice in the control group (3). After obtaining these results, the authors noted that this protein may be used to treat obesity, in addition to other diseases related to it, such as diabetes, liver disease, and some forms of cancer. Additionally, the study shows numerous other benefits of this protein (Figure 1):
- It lowers blood sugar and insulin levels, regardless of weight loss.
- It improves sensitivity of skeletal muscles to the effects of insulin.
- It reduces total fat accumulation by restricting fat deposit in the liver, kidneys, and blood.
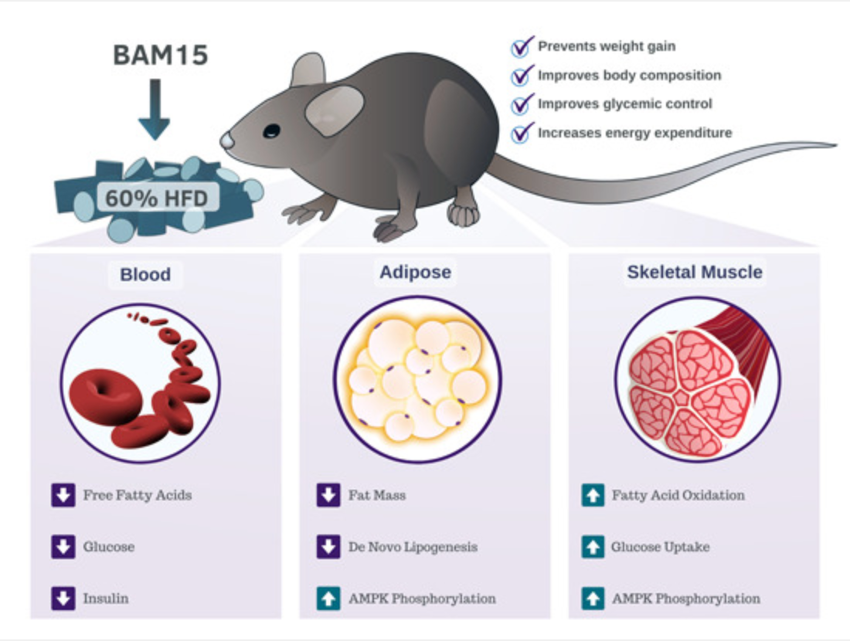
Generally speaking, BAM15 prevents weight gain, fat accumulation, and lowers blood sugar levels. Mitochondria burn more energy, and this way, the body composition and blood sugar levels of overweight and obese patients may be modulated. This compound is proposed as a treatment option for these patients, where scientists point out very good results in animal models.
Obesity is currently the result of a positive energy balance. The underlying causes of this positive balance are usually modifiable: a high calorie intake, a reduction in the body’s energy consumption due to decreased physical activity or, more commonly, a combination of both situations. Also, the socio-economic changes we’ve experienced in recent decades have led to a wider availability of food and the production of energy-dense and very nutritionally poor processed foods. At the same time, physical activity has been drastically reduced in the population, due to more sedentary work and the generalization of means of transport. Additionally, we need to add the neuro-hormonal regulation of energy metabolism, which plays a permissive role in the development of obesity (5,6,7).
Despite the search for new drugs and treatments to prevent obesity, there is solid scientific evidence pointing to the change in habits that a person must make to achieve a healthy lifestyle and prevent obesity. A healthy diet has proven to be the fundamental component in the treatment of obesity and should be part of a comprehensive program that includes behavioral therapy and physical exercise, with the aim of, beyond reducing body weight, changing lifestyle habits (5, 6, 7). Therefore, the FESNAD-SEEDO consensus states that the dietary management of obesity should (6):
- Decrease body fat while preserving lean mass to the maximum
- Takes place in the long term
- Be effective in the long run, maintaining weight
- Prevent future weight gains
- Include nutrition education that eliminates bad eating habits and mistakes
- Decrease cardiovascular risk factors associated with obesity (high blood pressure, dyslipidemia, prediabetes or diabetes mellitus)
- Improve comorbidities linked to excess weight (sleep apnea, osteoarthritis, neoplastic risk, etc.)
- Induce psychosomatic improvement with the recovery of self-esteem
- Improve functional capacity and quality of life
Finally, at Neolife, we’ve developed a comprehensive program for the health promotion and disease prevention of our patients. Our approach to obesity through medical and nutritional treatment is one of Neolife’s specialties, with the highest positive results. Looking ahead, the use of new facilitative treatments, such as the use of the protein BAM15, may prove promising to improve body composition and metabolic balance outcomes. We will, therefore, be on the lookout for the latest results of the clinical trials conducted with this protein.
BIBLIOGRAPHY
(1) (2020). “Obesity and overweight”. World Health Organization. URL: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
(2) Mayo Clinic. (2020). “Obesity: prescription weight-loss medication”. URL: https://www.mayoclinic.org/diseases-conditions/obesity/diagnosis-treatment/drc-20375749
(3) Axelrod, C.L. et al. (2020). “BAM15-mediated mitocondrial uncoupling protects against obesity and improves glycemic control”. EMBO Molecular Medicine e12088. URL: https://www.embopress.org/doi/10.15252/emmm.202012088
(4) (2020). “Mitochondria”. National Human Genome Research Institute. URL: https://www.genome.gov/genetics-glossary/Mitochondria
(5) Liliana P. Rodota y María Eugenia Castro. “Nutrición clínica y dietoterapia” [Clinical nutrition and diet therapy]. Editorial Médica Panamericana, 1ª Edición, 2012.
(6) De Luis Román, D.A. Bellido Guerrero, D. García Luna, P.P. Olivera Fuster, G. (2017). “Dietoterapia, nutrición clínica y metabolismo” [Diet therapy, clinical nutrition and metabolism]. Third Edition. Sociedad Española de Endocrinología y Nutrición. Grupo Aula Médica, S.L. Madrid, Spain.
(7) Redondo S., M.R. & González R., L.G. (2015). “Nutriguía: manual de nutrición clínica” [Nutrition Guide: Clinical Nutrition Manual]. 2nd Edition. Editorial Médica Panamericana.

