The energy and nutrients we obtain through food play an important role in the development and preservation of the immune system.
The nutritional approach to immune disorders should aim to maintain an optimal nutritional status, prevent deterioration during acute episodes, and improve it during symptom-free periods. The AESAN Scientific Committee Report shows that the immune system is strongly dependent on adequate and balanced nutrition.
Alejandro Monzó – Neolife Nutrition Unit
Relationship between specific nutrients and the pathogenesis, symptoms, and evolution of autoimmune diseases
The immune system consists of a network of specialized tissues, organs, cells, and chemicals that protect against infectious agents, toxins, cancer cells, and foreign tissues (1). There are many individual variations in immune functions caused by an individual’s genetic make up, nutritional status, stress levels, age, and lifestyle habits.
The immune system has several lines of defense. Early defense mechanisms aimed at combating and eliminating foreign elements involve physical, chemical, and biological factors, such as the skin barrier, mucous membranes, stomach pH, digestive enzymes, and others. When these mechanisms fail or are overloaded, innate and adaptive immunity take over (1, 2). Both interact with each other with the aim of preserving the body’s homeostasis. Innate immunity is the first to act, is natural and non-specific, does not require prior sensitization, is mediated by cells with phagocytic ability and (natural killer) cells and, by itself, allows the control of most of the pathogens that reach the body. Adaptive immunity is specific and has immunological memory when the body is exposed a second time to a given antigen, with priority participation of lymphocytes, and the antibodies and cytokines released by them.
In some people, the immune system is altered and finds it difficult to recognize its own cellular structures and tissues, so it initiates an attack against them. When this occurs, autoimmune diseases originate. Currently, over 80 diseases have been described and the autoimmune attack may be restricted to specific tissues or may be generalized, such as rheumatoid arthritis, lupus, type I diabetes, Hashimoto’s thyroiditis, Graves’s disease, celiac disease, Chron’s disease, multiple sclerosis, ulcerative colitis… (1, 2). In many cases, the reason why this happens is unknown; however, it is believed that the presence of some microorganisms, the ingestion of some drugs, toxins and/or certain chemical substances present in food may trigger this reaction, especially in the case of individuals who are nutritionally deficient or who have a greater genetic susceptibility to developing autoimmune disorders.
The development therefore, maintenance, and proper functioning of the immune system depends on adequate and balanced nutrition. According to scientific evidence, improper nutrition affects the innate and adaptive immune response, altering the response to infection, indirectly increasing the virulence of pathogens, and favoring the development of autoimmune diseases (Figure 1) (3). According to the previously mentioned AESAN (Spanish Agency for Food Safety and Nutrition), there are several reasons why the immune system depends on the availability of nutrients (1):
- The immune response is associated with the synthesis of new protein molecules and cell proliferation.
- Nutrients act as cofactors in many metabolic pathways that are critical to the maintenance of immune function. Moreover, they can regulate oxidative stress and cell membrane integrity.
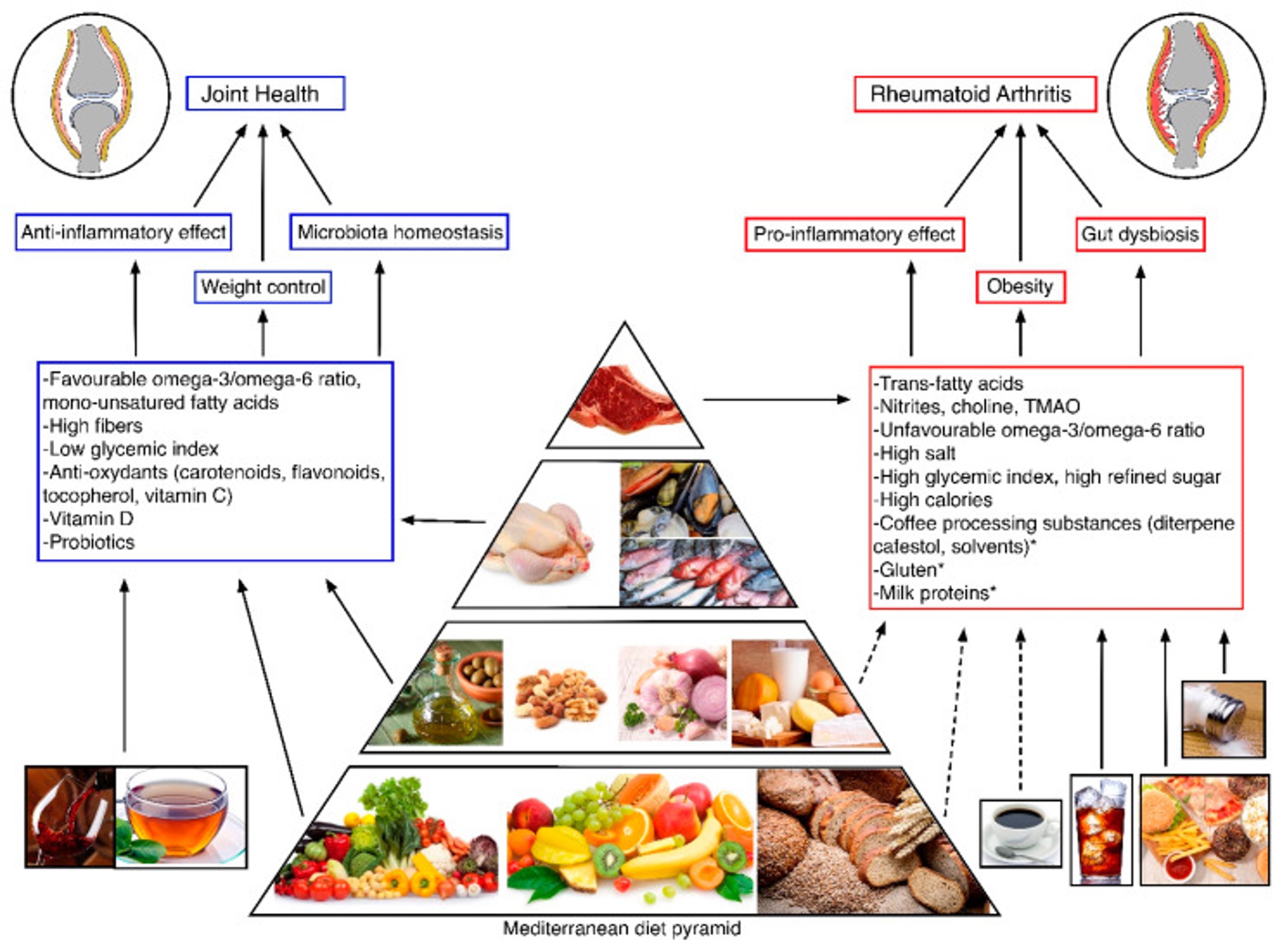
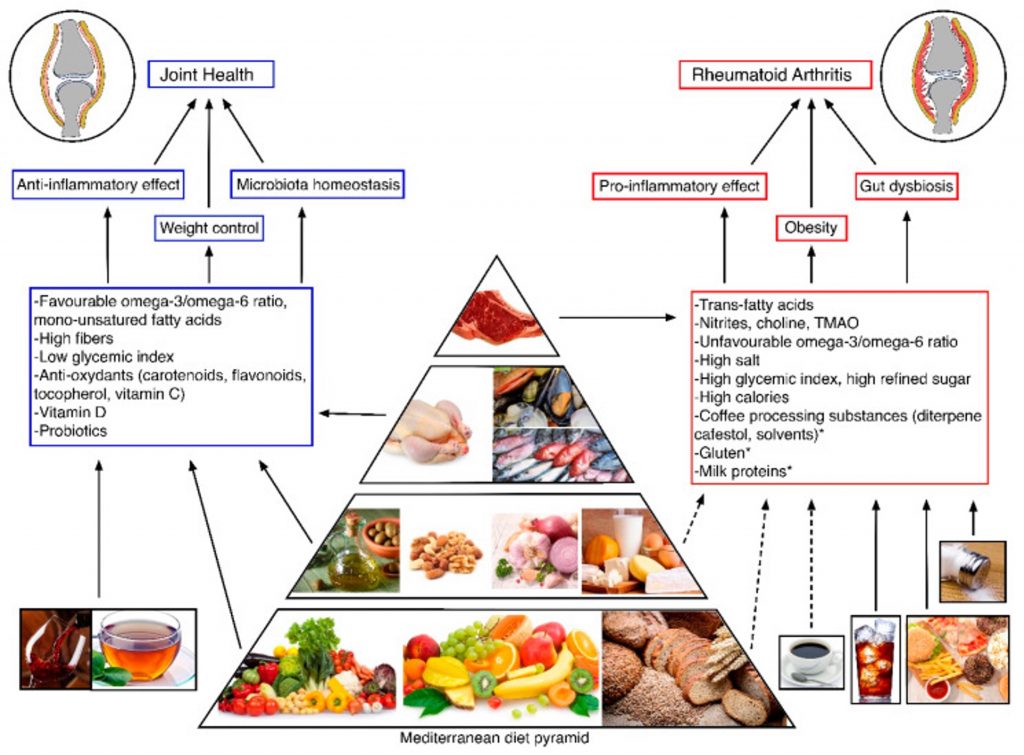
Figure 1. Nutrients and their dietary sources are involved in the development and progression of rheumatoid arthritis (3).
The cells of the immune system rely heavily on their cell membrane function to perform operations such as cytokine and antibody secretion, antigen recognition, lymphocyte transformation, and contact-dependent lysis. The importance of lipids in maintaining membrane integrity suggests that these compounds may be critical nutrients in immune regulation and, in fact, fats have been shown to influence the severity of autoimmune diseases (4). A diet rich in long-chain omega-3 fatty acids is recommended in this type of disease because of its relationship with inflammatory processes, its anti-inflammatory role and positive correlation with the increase in white blood cell levels, the patient’s weight, and improvement of cardiovascular risk, and so they should provide 1-2% of the total energy provided by food (1, 2, 3).
In experimental animal models of autoimmune diseases, certain nutrients (polyunsaturated fatty acids, vitamins A, E, C, D, and B12) and probiotics produce significant clinical improvement and delay in disease onset. In patients with autoimmune diseases, some nutritional intervention studies suggest that various dietary components, especially omega-6, 3, EPA and DHA fatty acids, vitamin D, and selenium, as well as the administration of various probiotics in combination, may have an impact on patients’ clinical improvement (1).
As nutritional recommendations to optimize our immune system, we present the following foods and nutrients, which play an interesting role in the modulation of immune response (4, 6, 7):
- Vitamin A: beef liver and other organs, salmon, green leafy vegetables, colorful vegetables, egg yolk, dairy products, and fruits such as melon, mango, and watermelon.
- Vitamin C: citrus fruits, as well as fruits and vegetables in general, red and green peppers, tomatoes, broccoli, kiwi, and strawberries, among others.
- Vitamin D: Vitamin D deficiencies are associated with increased risk of infection and autoimmune diseases. It is found in fatty fish, fish liver oils, egg yolk, cheese, and mushrooms along with adequate sun exposure and/or supplementation.
- Selenium: participates in the production of important agents in immune and inflammatory response, in addition to improving the activity of natural killer cells. It is present in seafood, Brazil nuts, meats, eggs and other dairy products, bread, and cereals.
- Zinc: its deficiency increases susceptibility to infections; this nutrient is involved in multiple processes of the immune system. Oysters, red meats, seafood, legumes like chickpeas, and nuts are good sources.
- Healthy fatty acids: fish and seafood, nuts and seeds, plant oils and fortified foods like dairy.
- Interesting foods: broccoli, garlic, turmeric, ginger, green tea and mushrooms, kefir, and probiotic foods in general; the immune system benefits from their immunomodulatory functions, preventing inflammation.
While regular moderate physical activity facilitates body weight control, improves vascular health, and generally supports optimal immune function, intense exercise is consistently associated with short-term immunosuppression. This effect, which lasts 3-72h, is apparently aggravated by a relative depletion of carbohydrates and is mitigated by their consumption before or during exercise (4). And so, a study published in Frontiers in Immunology points out that proper nutrition together with regular moderate physical activity may prevent the risk of obesity and may improve immune function (Figure 2.) (5). It is worth noting that the immune system also benefits from periods of fasting, which promotes cell regeneration and reduces inflammation (6).
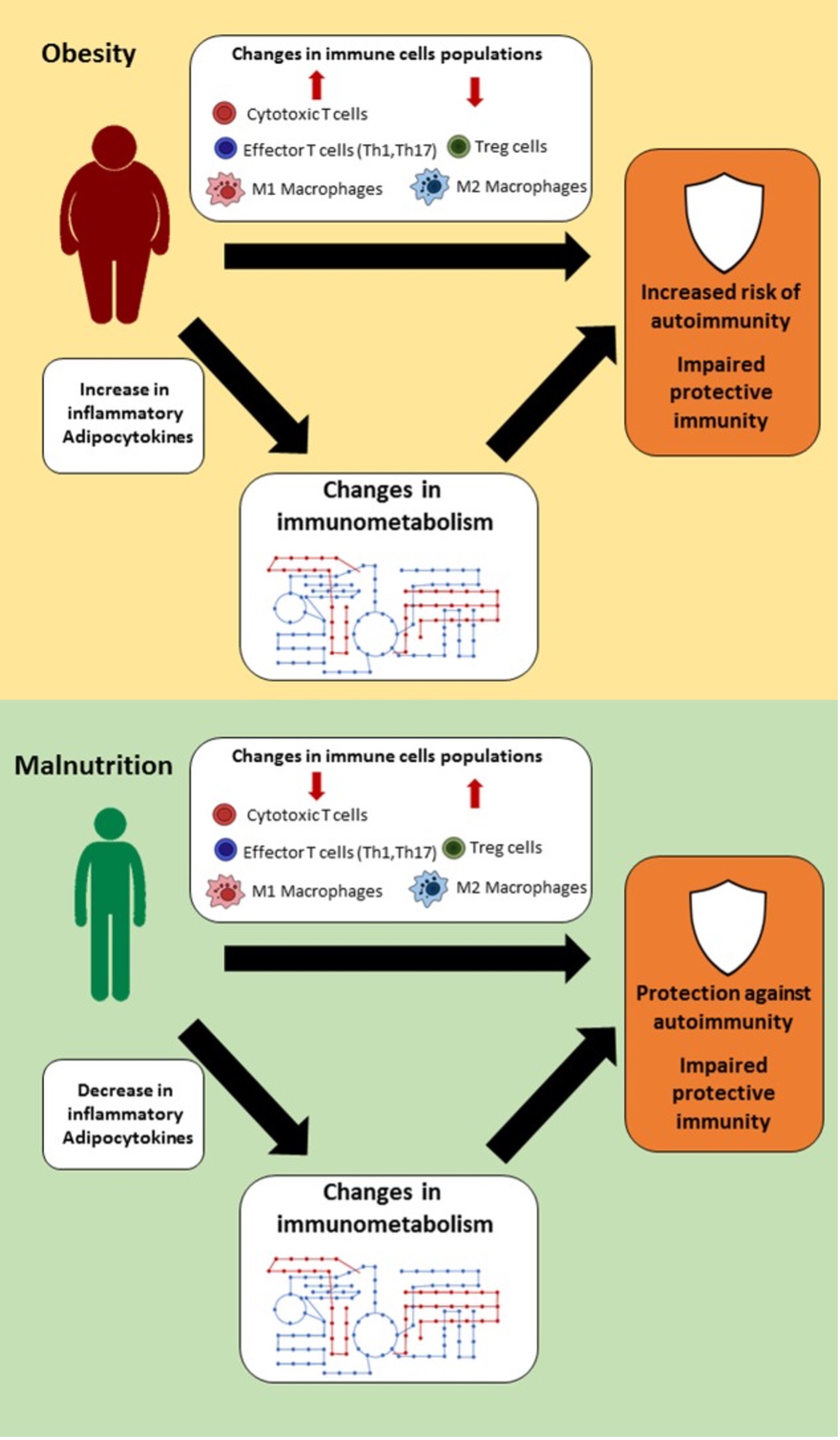
Figure 2. Link between nutritional status, immune metabolism, and immune function.
Finally, more and better quality studies are needed to better understand the impact of nutrition and nutrients on the pathogenesis, symptoms, and evolution of autoimmune diseases. In short, immunological disorders may be grouped into three major groups: allergies or states of hypersensitivity, states of immunodeficiency, and autoimmune diseases (1, 2). Here at Neolife, we prescribe a personalized nutrition plan based on the patient’s special needs. Following the latest advances in the scientific community, a diet can be an optimal tool, especially for the management of immune system disorders, which is why both medical and nutritional follow-up is essential in our clinic.
BIBLIOGRAPHY
(1) Report of the Scientific Committee of the Spanish Agency for Food Safety and Nutrition (AESAN) on the Role of Nutrition on Autoimmune Diseases. Scientific Committee Journal number 13. 2010. URL: https://fisiogenomica.com/assets/Blog/pdf/NUTRICION_ENFERMEDADES_AUTOINMUNES.pdf
(2) Plaza L. B. & Bermejo L., LM. (2017). “Nutrition and immune system disorders”. Nutr Hosp. Vol. 34(4): 68-71. URL: https://pubmed.ncbi.nlm.nih.gov/29156936/
(3) Gioia, C. et al. (2020). “Dietary habits and nutrition in rheumatoid arthritis: can diet influence disease development and clinical manifestations?. Nutrients.Vol. 12(5): 1456. URL: https://pubmed.ncbi.nlm.nih.gov/32443535/
(4) David L. Katz et al. Nutrición Médica 3ª Edición. Wolters Kluwer. 2015.
(5) Alwarawrah, Y. (2018). “Changes in nutritional status impact immune cell metabolism and function”. Front Immunol. Vol. 9: 1055. URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5968375/
(6) Vázquez, M. (2018). “Fortalece tu sistema inmune: mejores defensas = menos enfermedad” [Strengthen your immune system: better defenses = less disease]. Fitness Revolucionario. URL: https://www.fitnessrevolucionario.com/2018/05/26/como-fortalecer-sistema-inmune/
(7) National Institutes of Health. U.S. Department of health & human services. Dietary Supplement fact sheets. URL: https://ods.od.nih.gov/factsheets/list-all/